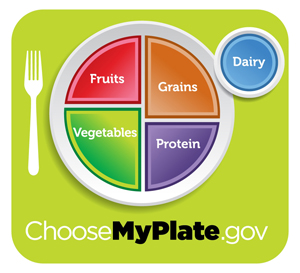
The new USDA public nutrition guidelines are being updated again, as scheduled, and the Dietary Guidelines Advisory Committee’s version now says some egg yolks are okay and to limit carbs and sugar instead. A variety of media commentators have jumped all over that, even though it’s not very different from what the guidelines have been emphasizing for years. Now, if anything, I would have hoped that most of the commentaries in the newspapers of record would be critical of the industry influence on the USDA’s nutrition guidelines for the general public each time, but no.
The most prominent commentators, notably Nina Teicholz, whose op-ed in last Sunday’s New York Times really bothered me, are well-educated and should know how to “read a french fry” as it were. But instead of looking at the likely effect of loosened USDA dietary limitations on a public that has gone so seriously overboard on calorie-dense food, they’ve taken the opposite tack. Mostly to declare self-righteously that the new relaxation of standards really means all the previous recommendations to limit saturated fat and cholesterol were bunk and a waste of time based on “uncertain” and “weak” or even “junk” science.
Which is untrue. Epidemiologic research–large observation studies and surveys, like the NHANES diet and cardiovascular health survey series from the 1970s onward, and the big Framingham Heart Study of the 1950s onward, are not junk science. They do what clinical feeding trials can’t: they look for the contribution of individual dietary risk factors to chronic and complex-origin health conditions like heart disease and stroke across very large population groups. Both the processed food industry and people like Teicholz claim that clinical feeding trials are the only legitimate way to provide “proof” of cause and effect, but the cost of conducting them carefully long enough and with a big enough participant pool for meaningful results would bankrupt the nation halfway through.
Epidemiologic findings matter on the large public scale. Not every specific applies absolutely and equally to every single person, but that’s not what population-wide studies are for. The big studies, loose as they might seem compared with DNA fingerprinting and perfectly demonstrated cause-and-effect kinds of lab workups for individual cases, give best-bet recommendations for most people to reduce their risk.
Your genetics determine how well that works for you specifically, but most of us don’t have access to DNA testing on that level, and the “big six” lifestyle risk factors (high sat fat, high blood cholesterol and blood pressure, overweight, lack of exercise and smoking) are a lot easier to change and get some control over. After all, you can’t change your genetics much (and yes, my daughter is quite disgruntled that she can’t pick cooler parents. But tough. We couldn’t pick ours either).
So anyway, I know I’m unusually irritated with any news about USDA dietary guidelines–I used to work at NIH, and some of my colleagues had attempted to serve on the dietary guidelines committee and ended up completely frustrated at how “bought” the process became. The USDA has always had a conflict of interest when it comes to public health recommendations because its main mission is support of US agriculture, and public health always comes a distant second to big business. The committees have repeatedly subverted and weakened the scientific nutrition panelists’ best-finding recommendations by including food industry participants and weighting toward industry priorities in the consensus mix. There’s no great reason to expect the food industry isn’t still playing and winning the same game on the same committee this time around. [Update: the meat industry has just asked for an additional 75 day comment period].
But the main problem I see at this point is how poorly mainstream journalists and editors have handled the announced overhaul. None really seem to have dug into the comparison between current and previous issues of the guidelines, much less compared the USDA’s final takes with dietary guidelines from the DGAC, a combined group of more purely biomed/scientific research experts representing HHS (including NIH) and the FDA, or those of the major health advocacy organizations such as the American Heart Association.
And declaring that it’s now fine for anyone to eat all fats without limitation is nonsense and a misread. The USDA guidelines don’t say that–the DGAC draft guidelines certainly don’t say that. And if the USDA does attempt to drift in that direction for the final release, as some of the director’s announcements suggest, given the participation of Big Food and Big Agriculture hoping to sell the public more meat, eggs, and cheese, along with more profitable processed goods, would you necessarily believe them?
Is it really the fault of the scientists on the panels over the years, as Teicholz claims (“How did they get it so wrong?”), that the epidemiology findings they relied on for previous rounds of recommendations weren’t borne out by much smaller and less conclusive clinical studies?
Maybe the role of saturated fat is less apparent in a clinical study. I don’t doubt that. But as noted above, the statistical power of the comparatively short-term clinical trials for cardiovascular disease effects is bound to be a lot lower than in a long-term population-wide study, even if the controls are tighter. There are so many interfering factors–other dietary and lifestyle factors, and so many varieties of genetic risk factors within and among different population groups, genders, and age groups, that you need the big numbers and the large timescale to see effects above the noise. Meta-analysis of a lot of limited clinical studies with iffy results doesn’t make up for that. If anything, it compounds their individual uncertainties.
[And in fact it turns out that much of Teicholz’s assumption on that point is based on a very poorly conducted, much criticized meta-analysis of studies on saturated fat and cardiovascular disease published last spring. Most inclusive meta-analyses performed using standard stats analysis best practices actually show reductions of between 14 and 26% in CV events and deaths when subjects cut their saturated fat intake below 10% of calories and ate more vegetables instead of carbs, or else substituted polyunsaturated fats for them.]
Teicholz’s op-ed had carefully modulated but still overt indignation at the imperfect scientific basis behind previous recommendations to cut saturated fat and limit egg yolks and other high-cholesterol foods. What should be there and isn’t is the acknowledgement that when those recommendations were first announced to the public–by the AHA, the CDC and the USDA in the late 1960s, population trend studies over the next 10 years showed a stark drop in the rate of heart attacks–about a 30 percent drop. In other words, it worked. Big time.
And the broad peak of the population curve for a first heart attack shifted to the right by 10 years–that is, the average age for men went from about 50 to about 60, and for women from about 60 to 70. These were huge improvements in public health overall, and they were achieved partly because the public believed and paid attention, and partly because the nutrition and health experts hadn’t given up and abdicated responsibility in the face of industry pushback.
Clearly these results didn’t last; but is that the fault of the studies that identified saturated fat and cholesterol as things to reduce (note: not eliminate completely, just reduce)? The 1980s ushered in a long Republican-led era of unfettered, uncritical support of corporate priorities over public health, Reagan’s “ketchup is a vegetable” quip and the conversion of school lunches to chain restaurant concession contracts, a popular nose-thumbing at so-called “food police” health recommendations, the rise of high-fat-and-sugar-and-oversized-portion “comfort” and “indulgent” foods in restaurants and food magazines, and an entrenched anti-science bias in Congress that still haunts us today.
Not that much has changed from Reagan’s time in office–including the sad observable fact that most Americans for the past decade or so clearly aren’t paying serious attention to or even attempting to follow those modest earlier USDA recommendations, particularly the recommendations to eat more vegetables rather than more boxed, labeled namebrand processed foods, whether Big Macs or Ding Dongs or Froot Loops…
So few Americans today eat any vegetables at all compared with people of the same ages in the 1970s. As I’ve mentioned before, a shocking number of my friends, in their 40s and 50s already, do not cook at all. They have advanced degrees, if mostly in the humanities. They nervously repeat but don’t understand how to read between the lines of whatever diet and health claims are in the news, and they’ve come to think cooking is too hard. They have a lot of takeout menus on their iPhones.
There is just one more factor to mention here: the profit motive. Teicholz, a former contributor to NPR, Gourmet and Men’s Health, wrote that op-ed in part to promote her new book, The Big Fat Surprise, which claims that diets high in meat, butter, Continue reading →
Filed under: books, Diabetes, Food Politics, history, meat and poultry, nutrition, unappetizing | Tagged: AHA, cardiovascular disease, Nina Teicholz, public health, USDA dietary guidelines | Comments Off on Media misread on the new USDA dietary guidelines